Robotic Prostate Cancer Surgery
Prostate cancer surgery performed using Robotic System is called ‘’Robotic Radical Prostatectomy’’.
Patients diagnosed with only inner gland prostate cancer were being operated on using conventional open surgical procedure, which provided total removal of prostate. But since 2000, laparoscopic radical prostate surgery has started to be performed worldwide. However, because of seriously long and challenging learning curve and performing periods, nowadays it can only be performed by a limited number of surgeons.
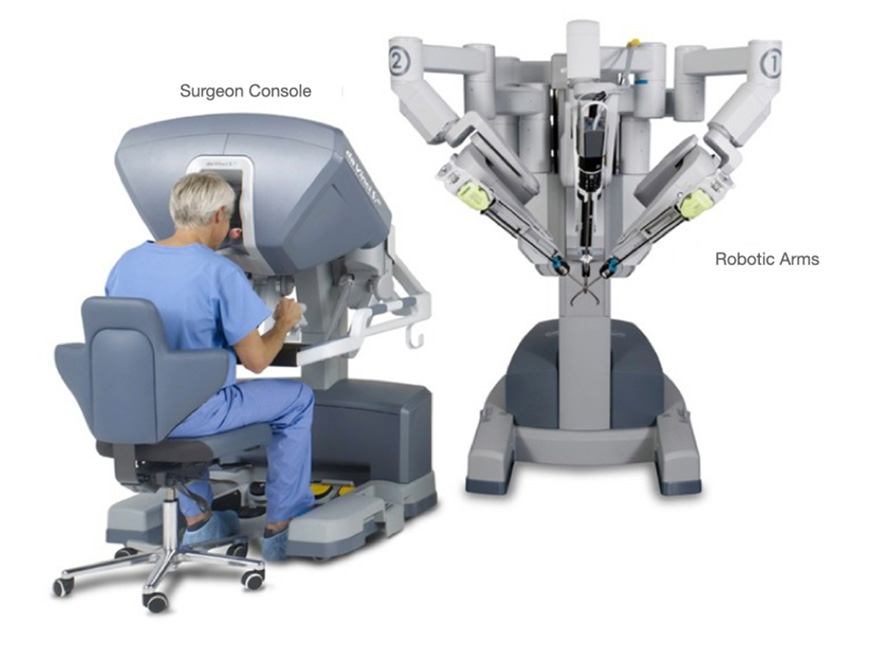
This surgical technic -Robotic Surgery using daVinci Robot-, which has offered many advantages following the developments in hardware-software systems and imaging technologies, has started to be used especially in the treatment of prostate cancer, thanks to the significant worldwide developments since 2002.
Nowadays, in USA, more than 95% of prostate cancer surgeries are being performed with the help of robotic system.
Main surgical steps carried out during Robotic Surgery are similar with the steps in conventional laparoscopy. In scientific literature, robotic surgery is mentioned as Robot-Assisted Laparoscopic Surgery. Thus, a surgeon’s advanced previous laparoscopic experience may play an important role in the success of the surgery, when compared to a surgeon performing only open procedures, and who takes the first step to robotic practices without any laparoscopic experience.
Surgical procedure in Robotic Surgery is performed via robotic arms controlled by the surgeon, with the help of a high-definition three-dimensional (3D) vision system that magnifies 10-15 times and robotic arms that are placed into body through small trocars. The biggest advantage of these robotic arms is, thanks to their thin and tiny ends, they enable the surgeon to perform the surgery multi-directionally by maneuvering the robotic arms with total 540 degrees of articulation in three dimensions and three directions, without any tremors.
During the operation called Radical Prostatectomy, which is performed for surgical treatment of prostate cancer, just after the removal of the prostate, urethra is sewn back to bladder neck at the level of the outer urinary sphincter to restore the continuity of the urinary canal as you can see in the above image.
Image-1: Operating theatre set up of daVinci Robotic System’s three components as a whole.

Image-2: The ‘’Console’’ used by surgeon to control daVinci Robotic arms.
daVinci Robotic Surgery Through a Single Hole
In recent years daVinci Robotic Surgery, though in limited numbers, can be performed through a single and tiny hole (3 cm’s) in the belly (but in only a few centers around the world).
Today, prostate cancer surgeries are not routinely being performed through a single hole. This single port daVinci Robotic Radical Prostatectomy can only be used on a very limited number of patients, only in several centers.
Thanks to this technique there is no need to make extra incisions to place 3 robotic arms into the body; the 1.5 cm’s incision in the belly through which the robot camera is placed into body is being extended 2 more cm’s and robot arms are being inserted through this stretched incision, via a special system (Image-3a). Robot arms are placed into body through only one hole on the belly, instead of 4 different holes (Image-3b).
Image-3a: Appearance of the robot arms that are placed into body through belly button.
Image-3b: The port with 3 holes (SILS Trocar) is being placed into body through 2cm’s wide single hole on belly. Robot arms are being inserted through this single hole.
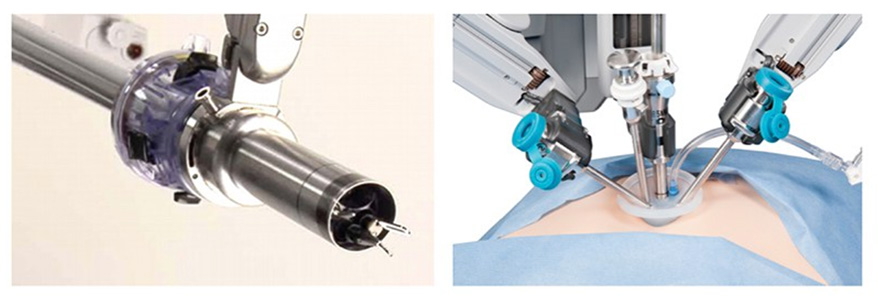
For a surgeon, the hardest part of performing that kind of a complicated operation with the help of robot arms placed into body through a very narrow hole is that this procedure requires patience, attention and extensive experience. However, thanks to the technological progresses, these disadvantages can be overcome with the help of the wide angle provided by robot arms that can extend like octopus tentacles after being placed into body.
Extraperitoneal Robotic Surgery
What is Peritoneum?
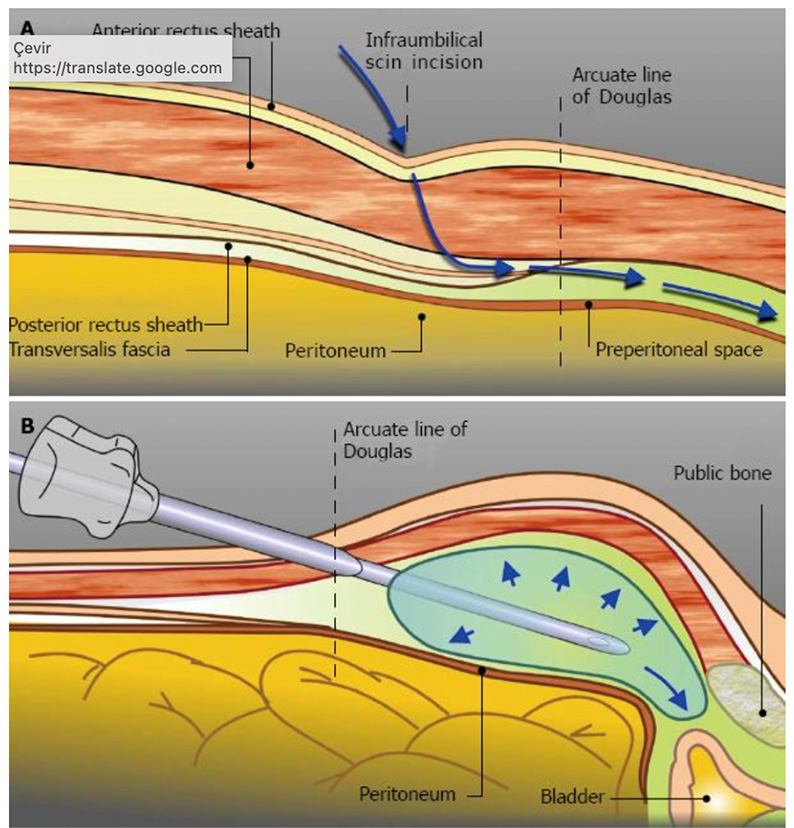
Peritoneum is a membrane made up of two layers, which lines the abdominal cavity completely. It is a protection mechanism that covers and provides support to the organs such as stomach, bowel, liver and spleen, and prevents their contact with outer environment. In addition to holding these organs together, peritoneum provides protection not only structurally, but also by the contents of the special peritoneal fluid it secretes (Image-4).
Image-4: Abdominal peritoneum is a protective membrane that encircles liver, stomach, duodenum, small and large intestines. Kidneys, bladder and prostate reside outside the peritoneum. Technically it is easier to reach these organs by piercing through peritoneum. However, in that case the tissues covered by peritoneum are directly affected by the surgery and will be in the risk area.
What is Extra-Peritoneal Robotic Surgery?
In every center of our country and in most centers around the world, daVinci Robotic surgeries are being performed by entering into abdomen through peritoneum and operating just next to intestines, stomach and liver. This is called ‘’Transperitoneal Robotic Surgery’’. The most important thing to be known is: Prostate, kidneys and bladder are the organs that reside in the outer part of peritoneum (Image-4). In Turkey, Prof. Dr. Tibet Erdogru performs Robotic Radical Prostatectomy without cutting through or damaging peritoneum by perforating, touching intestines or other intraperitoneal organs. During ‘’Extraperitoneal’’ Robotic Surgery, 1.5 cm’s incision is made below belly button. Since this incision is on the belly button line, the possibility of an unwanted scar from the incision can be minimized (Image-5).
Image-5: Small incision below the belly button
In an operation that is performed with ‘’Extraperitoneal’’ approach, entrance is made through belly button, between muscles that form anterior abdominal wall and peritoneum that encircles intestines – without opening the peritoneum. A special ‘’Balloon’’ placed in there creates a space and thanks to this procedure, robotic surgery space becomes ready for the operation to be performed easefully, without opening peritoneum and touching intestines (Image-6a, -6b). This technique is called ‘’Extraperitoneal Robotic Radical Prostatectomy’’.
Today, the reason why many medical centers adopt Transperitoneal technique is their necessity to do so. Usually, these centers which have a habit of performing open surgeries and do not have laparoscopy experiences, or which start performing robotic radical prostatectomy with no previous open surgery experiences, are being obliged to adopt Transperitoneal approach. The most important factors for being able to prepare the Extraperitoneal area are having an extensive experience in laparoscopic radical prostatectomy and possessing the necessary experience to perform this procedure extraperitoneally. Because, when extraperitoneal technique is desired to be performed by an inexperienced specialist, in case of the perforation of peritoneum which is very thin, the gas that is insufflated into body will release into peritoneum and this perforated peritoneum along with the displaced intestines will make the surgery much more complicated. For these reasons, preparing extraperitoneal area and performing Robotic Radical Prostatectomy in this area requires so much previous laparoscopic experience.
Image-6a: A cavity is created with a balloon to perform the surgery between anterior abdominal wall muscles and peritoneum (blue line), without touching intestines.
Image-6b: Creation of extraperitoneal cavity via the balloon inserted through belly button, in order to perform the surgery without putting intestines at risk
Based on the comparison of our experience with our latest Robotic Prostate Cancer Surgery cases (100 transperitoneal and 100 extraperitoneal cases), we found out:
- while there is no difference in terms of operation time and blood loss,
- it was worth of notice that the patients operated with extraperitoneal approach did not have gas pains and only 5-6 hours after the operation they started oral feeding and drinking water. In our country, there is no other comparable series of experiences that can be put forward. Thanks to this experience, we can say that post-op period is more comfortable for patients operated by extraperitoneal approach.
Differences between Robotic Radical Prostatectomy in Prostate cancer by extraperitoneal approach (without entering peritoneum) and by transperitoneal approach (by entering peritoneum and touching intestines) are listed below:
Advantages of Extraperitoneal Technique:
- Since there insufflation is made in the extraperitoneal area, intestines are not put under direct pressure throughout surgery and bowel movements start much sooner after the operation.
- Since there is no contact with intestines, and peritoneum integrity is preserved, there is no risk of bowel perforation.
- Since the peritoneum is opened during transperitoneal operations, intestines always get in the operating area in the course of prostate surgeries. In order to minimize this, during transperitoneal operations patients must be placed in a 45 degrees head down position throughout the operation. However, during an extraperitoneal surgery peritoneum is not being opened and since the necessary operational cavity is being created outside the peritoneum by insufflation, intestines never get into the area of surgery. Thus, patient is not placed in head down position. Patients are tilted in a small degree, which is nearly horizontal. (Image-7)
- Thanks to this kind of a positioning, there is exactly no possibility of brain edema and extra pressure to the heart caused by increasing blood flow.
- In case of an infection or urinary leakage, liver is not affected.
- Operation is performed through only 5 trocar holes (Image-8). When the largest trocar is inserted through belly button line, possibility of scar remaining is very low with this approach.
Image-7: You can see the lying position of our ‘’Extraperitoneal’’ Robotic Surgery patient. Black line is parallel to the ground level; red line indicates the angle patient is placed. During the generally performed ‘’transperitoneal’’ technique, patient is placed at the angle shown with white line – which is 45 degrees head down.
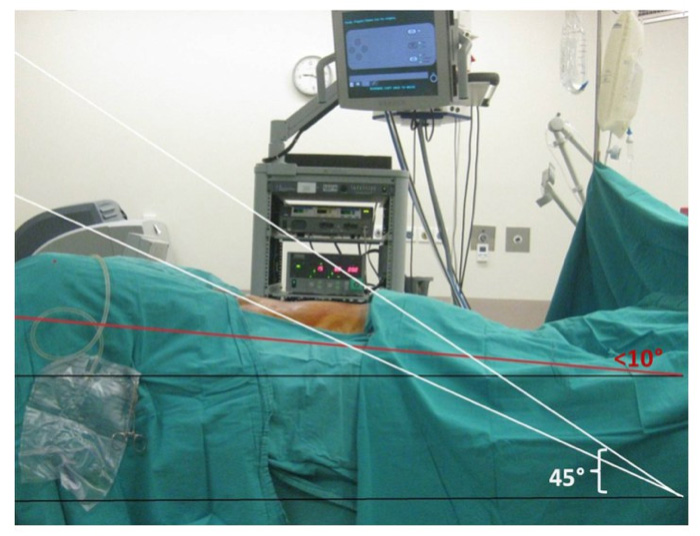
Black Line: Ground level
Red Line: Patient positioning angle during Extraperitoneal technique
White Line: Patient positioning angle during Transperitoneal technique
Image-8: While performing Extraperitoneal technique, usually 5 trocar holes are being made. The trocar you can see in the middle is a special one that is placed on the belly button, produced especially for extraperitoneal technique.

Disadvantages of Extraperitoneal technique:
- While performing a robotic surgery without entering the peritoneum, surgeon’s working area is much smaller. For this reason, in addition to an experienced surgeon, this procedure also requires high level of surgeon – surgical assistant accordance and experience.
What are the advantages of Robotic Surgery in Prostate Cancer?
After ‘’Robotic Surgery’’ patients stay at the hospital for 1 or 2 days. About 95% of the patients go back their home on second post-operative day.
- When compared to conventional open surgery, blood loss during operation is considerably lesser. In parallel with this, blood transfusion percentages are lower (1-2% for robotic surgeries, 40-45% for open surgeries).
- Patients need to take very few painkillers during hospitalization period and at home following their discharge. And these painkillers are not the ones stronger than paracetamol.
- Generally, within the first week following the operation, if there are no complications in the recovery phase, catheter placed into urinary tract can be removed between 4th – 7th post-op days. For the patients operated with open surgery technique, catheter is removed generally between 14th-21st post-op days.
- Nearly 90% of the patients can get back to their work routine on the second or third week after Robotic Radical Prostatectomy Surgery.
If you are diagnosed with localized prostate cancer -in other words, if cancer has not spread to outside of prostrate and it does not have aggressive features- and if you do not have any other serious illnesses, you are a candidate for undergoing surgical treatment.
If you have received internal or external focal therapies (brachytherapy, HIFU) for prostate cancer, however, cancer could not be get under control, you are not a candidate for undergoing surgical treatment because of the harms caused by radiotherapy received.
If you have an uncontrollable blood disease, you are not a suitable candidate for prostate cancer surgery. Except these two points, radical prostatectomy via ‘’Robotic Surgery’’ can be performed on every patient.
Nerve-Sparing techniques in Robotic Surgery
We know that the nerve reaching out to penis, which provides erection during sexual intercourse is not a single one, but a bundle of nerves. However, latest studies indicate that in 60% of patients, this bundle is not localized at the bases of the lateral parts of the prostate (Image-9). This means, during an open surgery most of the surgeons cut the nerve bundle that lies on the anterior aspect of prostate, while supposing that they are protecting the nerve reaching out to penis. And even if the surgeon claims he has protected the nerves, contrary to their expectations patients are faced with loss of erectile function after the operation. Prostate, which is located below the anterior part of the pelvic and at the root of the penis, resides at a very deep point of body. However, laparoscopic technique has wiped out this disadvantage. Surgeon can see all the anatomical differences, all tissues lying in the deep parts of the body and operate on them, thanks to the high resolution and 10-15 times magnified view by a telescope and other thin ended, oversensitive surgical equipment inserted into body through belly. With the help of this display system and thin ended – oversensitive equipment, nerve and vein bundles can be perfectly protected in all cases. With help of daVinci Robotic Surgery, these advantages of laparoscopic surgery went one step further; thanks to this system, laparoscopist surgeon can perform operations with 3D and higher resolution displays, with the multi-directional movements of very thin and sensitive ends of robotic arms placed in the body, and with no tremors. This also enables surgeon to reach the tissue from every angle.
Image-9a and -9b: In image-9a, contrary to previous belief, nerve bundles are extending also lengthwise on the lateral surface of prostate in the 60% of men (black arrows). In image-9b, we can see nerve bundle is gathered in only one area in 40% of men, like in the common belief (shown with striped arrows).
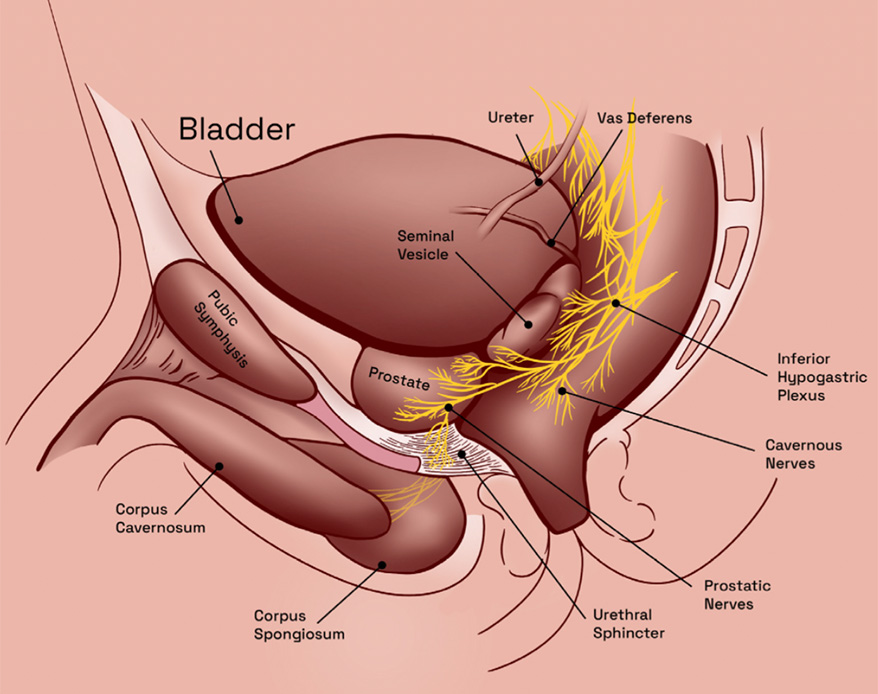
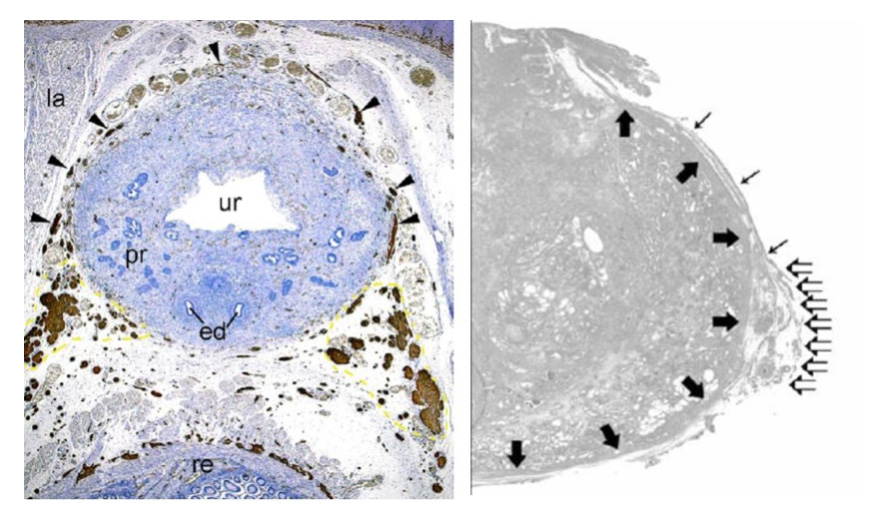
The nerve bundle reaching out to penis covers the posterior surface of prostate in 60% of men (Image-9a). Nowadays, nerve bundle and plexus are being spared via two different techniques. Performing this operation by keeping prostate capsule in its place and protecting both fascia around prostate and the nerve bundle + plexus located in the fascia requires ultimate experience and patience. This technique is called INTRAFASCIAL NERVE SPARING TECHNIQUE, which means from beneath all fascias (Image-10: Shown with red line). This technique is also named ‘’Veil of Aphrodite’’, owing to the view of fascias and nerve bundle in it that become visible while performing this technique. It is reported that after robotic surgery with this technique, penile erection is preserved 90-95%; but when conventional laparoscopy is performed via this technique, patients’ penile erection rate is around 85%. However, it is reported that, this rate is between 51-60% for patients undergoing open surgery.
If fascia covering the very upper part of the prostate capsule is left in its place, and not all the veil covering prostate thoroughly, but only the outer fascia on the sides and lower part of the prostate is preserved, this is called INTERFASCIAL technique – which means the technique performed from between fascias. With this technique, even when Robotic System is used, erectile function preservation rate is known to be 66%.
CLICK for Video of Robotic Intrafascial Nerve Sparing Surgery performed by Prof. Tibet Erdogru.
Image-10: Anatomical view of the nerve bundle reaching out to penis, and how it is being preserved during prostate surgery.
In Image-11, INTERFASCIAL and INTRAFASCIAL differences in preservation of neuro-vascular bundle located between fascia leaves are tried to be shown much more clearly. As it can be seen in Image-11a, with interfascial technique, neuro-vascular bundle between two fascia leaves are being preserved; in Image-11b we can see that with intrafascial technique, neuro-vascular bundle between two fascias on the prostate surface can be preserved as a whole.
Image-11a and 11b: Schematic view of the differences between interfascial and intrafascial nerve sparing techniques.
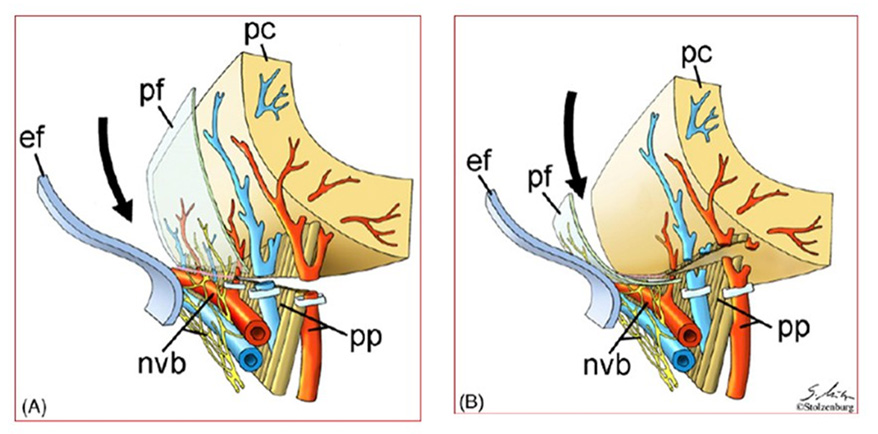
The most important point here to be emphasized is, in patients whose fascias with all layers and nerve bundles that provide penile erection are preserved totally -in the shape of Veil of Aphrodite-, continence function can also be regained up to 98% and much faster.
To sum up very briefly, thanks to the technical advantages of Robotic System and ultimate surgical experiences in laparoscopy, nerves and veins reaching out to penis can be preserved at a remarkable level and an important advantage is provided in terms of continuation of sexual activity postoperatively.
Urinary Muscle Preservation Via Robotic Surgery:
All technical Details:
Thanks to the experience we gained through conventional laparoscopy surgeries (without robot) in the surgical treatment of prostate cancer, we have been able to have a good grasp of anatomical details of many structures around prostate that we had not been able to see and make sense of while performing open surgeries. Studies in this subject are still being carried on. Especially the high-resolution and three-dimensional image display of the Robotic System provides us with supplementary information, following the previous details we gained thanks to laparoscopy. It should come as no surprise that these details cannot be seen by surgeons performing open surgery. Because, all the anatomical details that can be told reside at the root of penis, which is located under a bone we call pubic bone. In other words, this structure lies in one of the deepest parts of body.
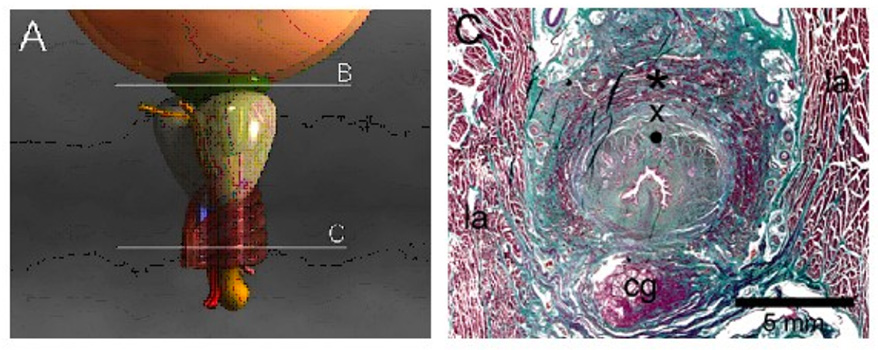
Full urinary control with protection of external sphincter (yellow star) and prostatic urethra (white dot) during robotic radical prostatectomy of our surgeries.
As we can see in Image-A, prostate is located just below the bladder. In this image, there is a double layer sphincter muscle fascicle embracing the part of the urinary canal which can be seen on ‘’C’’ cross section
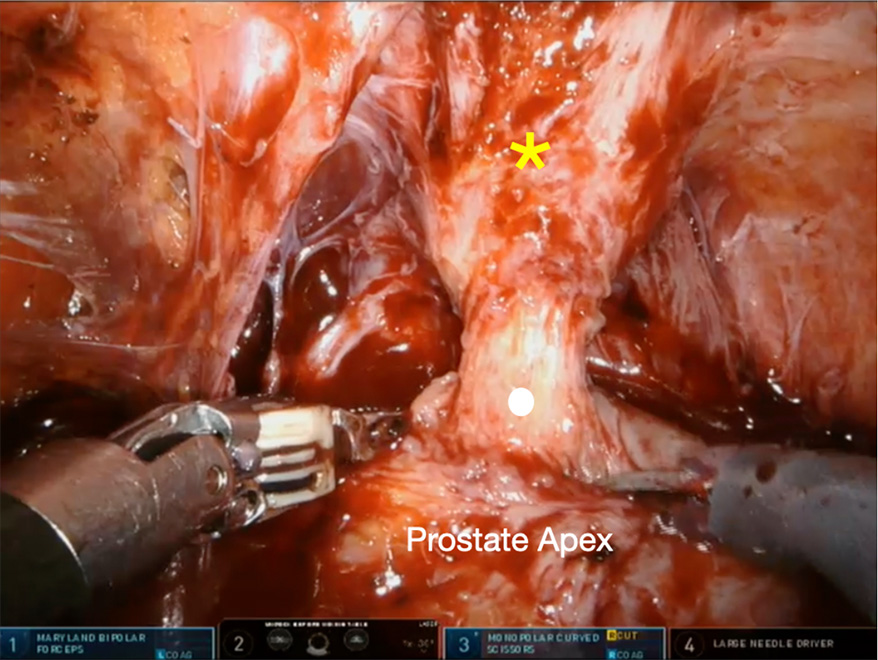
level. The one indicated as * is the strained sphincter muscle fascicle; X is the smooth muscle fascicle.
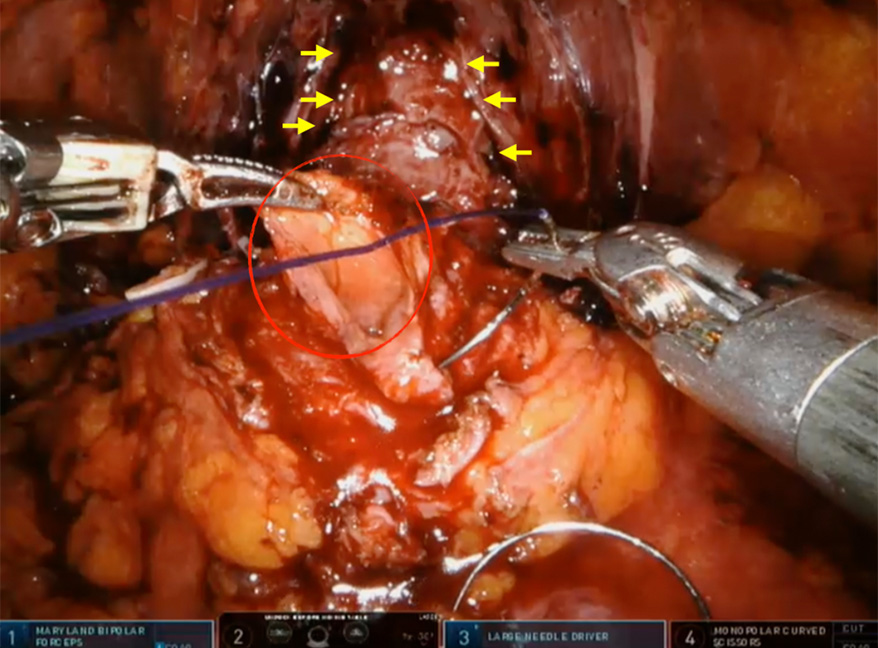
We also bladder neck sparing robotic surgery for excellent urinary control after the surgery. Red circle: Spared bladder neck, yellow arrows: bilateral sparing of neuro-vascular bundles for erection.
We can show this with a more detailed diagram:
Details of the urinary sphincter, which we had been able to acquire thanks to Robotic Surgery Technique, can be easily seen and preserved like you can see on the video (Click HERE for the video).
During Robotic Radical Prostatectomy surgery, owing to the advantages offered by robotic technology and the experience of surgeon, these muscle fascicles and nerve bundles can be preserved in a very delicate
way, without harming their structures. And this preservation offers patients faster continence regain and a high life quality without any loss in sexual function.
What are the Side Effects and Complications?
Evaluations carried out until today show that, urinary incontinence and erectile dysfunction problems which may occur following radical prostate surgery are encountered less frequently after laparoscopic prostate surgery.
With high definition and 10-15 times magnified display of a deep-seated organ like prostate, provided by the telescope used in Robotic System, and thanks to the very small robotic arms which do not tremble and which are capable of 540 degrees motion, Robotic System offers better preservation of urinary sphincter and of the nerves that facilitate penile erection and urinary sphincter. This kind of a remarkable preservation offers lesser urinary incontinence problems, and patients experience erectile dysfunction at lesser rates. If you are younger than 60 and you have undergone a bilateral operation with nerve-sparing technique, following your radical prostatectomy surgery via Robotic Surgery you can resume your sexual activity at a rate of 80-90% without any need to receive extra treatment. In addition to that, normal urinary continence rates are between 96-98%.
In the light of these information it can be better comprehended that the most important point to be known by patients and patient relatives is, Robotic Surgery technique is not a surgical practice that is dependent only upon the device and the robot. Depending upon my own experiences I can say that, a surgeon’s experience especially in conventional laparoscopy in radical prostatectomy plays an important role in the success of surgery. Let’s try to think of the success of an experienced surgeon who can easefully perform laparoscopic surgery despite its complexities and disadvantages – without the advantageous help of robot, performing this operation with the additional help of robotic technology, by preserving nerves and veins reaching out to penis and the urinary sphincters. Because of the great expectations of the patients planning to undergo this high technology operation, we believe that a surgeon’s laparoscopic experience is a factor that should exactly be questioned.
Getting Ready for Robotic Radical Prostatectomy in Prostate Surgery
Prior to the operation, condition of prostate cancer must exactly be evaluated in detail by medical imaging methods (examination by inserting a finger into rectum, prostate MRI, pelvic CT or with additional whole-body bone scintigraphy) in order to see whether it is limited in the prostate capsule, or extended outside the prostate capsule, or spread to the seminal glands and lymph nodes.
Data gathered form these examinations is evaluated by Prof. Dr. Tibet Erdogru via MSK Nomogram, and then with attendance of patient and relatives, a second – more detailed – evaluation is being made about the condition of the cancer and surgical expectations.
These data received, together with the number of biopsies on patient’s pathology report and his Gleason Score should be evaluated very carefully after patient arrives for his checkup. Only after this detailed evaluation process, in the presence of patient, a treatment can be planned. Laparoscopic or Robotic radical prostatectomy is one of primary surgeries in urology practice in terms of complexity and delicacy. Especially, how the surgeon will balance between the nerve-sparing technique and necessity of removing cancerous tissues totally while preserving the nerves, all other options and potential complications must be talked over thoroughly. In case of coming across to an unpredictable finding, it might be necessary to change the approach during surgery; or again, during the operation we may have to benefit from Frozen Section biopsy method to find out if there is any cancerous tissue is left on the spared nerve and vein bundles. Discussing these in great detail prior to the operation is very important for patient’s acceptance of the possible future treatments and for overcoming the disease.
If you are a regular smoker, you must quit smoking before this operation.
Necessary general anesthesia preparations to be completed within the preoperative 10-15 days:
- Complete urine analysis
- Complete blood count
- ECG (Electrocardiography)
- Serum fasting blood glucose, creatinine, liver function tests (ALT, AST, GGT), electrolytes (sodium, potassium, chloride)
- Chest X-ray (optional, if necessary)
If you are using blood thinner medications, you have to stop using them at least 7-8 days prior to the operation date given to you. If stopping these medications is forbidden, you must certainly get into contact with me. We have to make essential arrangements in order to avoid any delays in your treatment, or any risks in terms of operation. Since we perform the operation under general anesthesia, you should not consume any solid or liquid food 6 (six) hours prior to the operation.
Prof. Dr. Tibet Erdogru
Treatment of prostate, bladder, kidney and testicular cancers with robotic and laparoscopic surgery in urology

