Overview
Symptoms of chronic pelvic pain compound specialists in urology, gynecology, neurology, colo-rectal surgery, pyschiatry, pain management as algology. Pudendal neuropathy is a polysymptomatic phenomenon causing chronic, nonmalignant pelvic pain. In its simplest form, pudendal neuropathy causes perineal pain (pudendal neuralgia) that is aggravated by sitting or driving, reduced when standing, and relieved by sitting on a toilet seat. Despite repetitious complaints of pain and organ dysfunction, the diagnosis of neuropathic pain is delayed for years because evaluations and treatments are focused on suspected morphologic causes. Pudendal Nerve Entrapment Syndrome is a condition that can significantly impact daily life, causing chronic pain in the pelvic area.
This article will break down what PNE is, how it’s diagnosed, and the treatment options available, with a special focus on an innovative laparoscopic and robotic surgical methods firstly developed by Prof. Dr. Tibet Erdogru since 2010 (for 25 years)
Incidence
Few clinicians specifically interested in for pudendal neuralgia, so the incidence and prevalence are uncertain. Prevalence is calculated as 1% in a general population to 20% in a urologic and gynecologic practices in females. Chronic Pelvic Pian is common, affecting 8-9% of urologic office evaluations. The prevalence of chronic prostatitis, which may reflect pelvic neuropathic pain, has an incidence 3%. In our practice, the age at symptom onset ranges from a 17-year-old boy to a 83-year-old female.
Causes (Etiology)
Pudendal neuralgia (neuropathy) is a cumulative and repetitive trauma syndrome due to compression, stretch and direct trauma. It is typically an acquired problem due to repetitive micro trauma. The most seven most frequent causes are
Identified Reason | Activities |
Prolonged sitting | Computer tasks, long automobile or airplane trips (truck drivers, salesman, delivery persons) |
Pelvic surgery | Incontinence or other gynecologic surgeries (especially using mesh) Radical pelvic surgeries in males or females Complications due to pelvic surgeries as hematoma, infected urinoma etc. |
Cycling | Bicycle seat, distance of cycling, number of pauses |
Pelvic Trauma | Falls, motor vehicle accidents, motocross, horseback riding, sexual toys. |
Adult Sports or Exercises | Abdominal crunches, leg presses, weightlifting, spinning, stair climbing, volleyball, soccer, hockey, basketball |
Traumatic chithbirth | Duration of second stage of labor, large-size infant |
Constipation | Usually prolonged over many years. Constipation may be the cause or result in pudendal neuropathy |
The reason is not limited to these processes; for example, pelvic radiation therapy resulting in neuropathy of the pudendal nerve is infrequent but devastating. For last 20 years, the use of mesh during incontinence surgery has become the most common cause in gynecology.
Psychiatric illnesses do never cause CPP; however, psychosocial problems are common among CPP sufferers. In many cases, emotional dysfunction follows several years of misdiagnosis, repetitive non-specific antibiotic treatment, different tests, ineffective interventions and disrupted lifestyle. Disruption of the social network often requires psychological or psychiatric consultation.
Pathogenesis and Pathophysiology
Clinical symptoms suggest that pudendal neuropathy is mainly a disorder of small, unmyelinated C fibers affecting both somatic and autonomic afferent and efferent nerves.
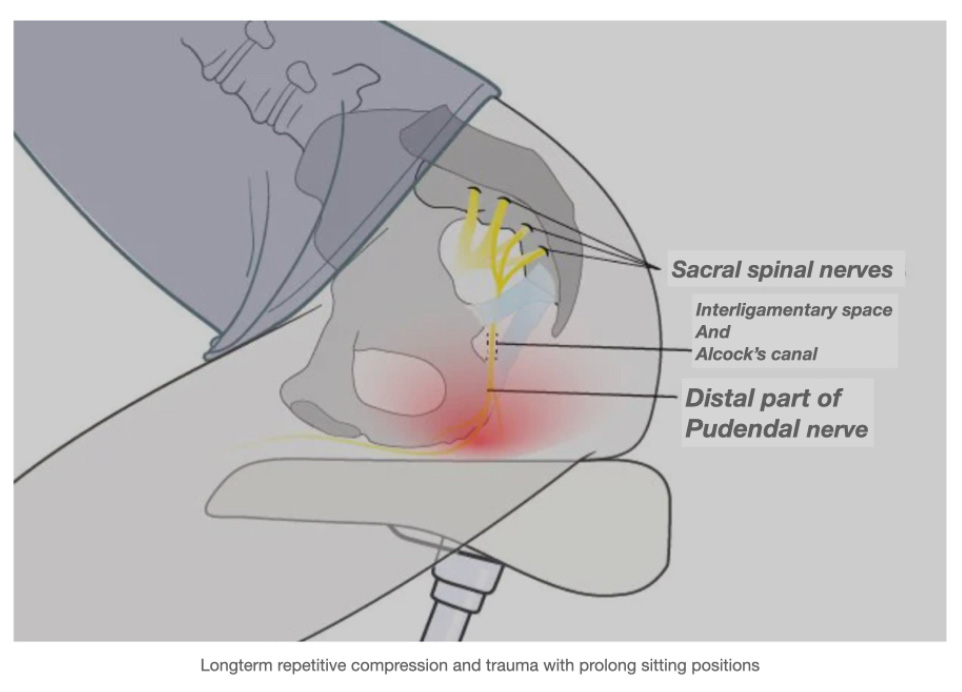
As mentioned before, causes of pudendal neuropathy include compression, stretch, direct trauma, and iatrogenic interventions such as pelvic surgeries (especially using with prolen mesh) and radiation. A common concern among patients is repetitive exaggerated flexion at the hip during running, cycling, exercising, and sports activities. Repetitive compression on the perineum while sitting on a bicycle seat exceeds by two-fold or three-fold pressure resulting in temporary neural ischemia.
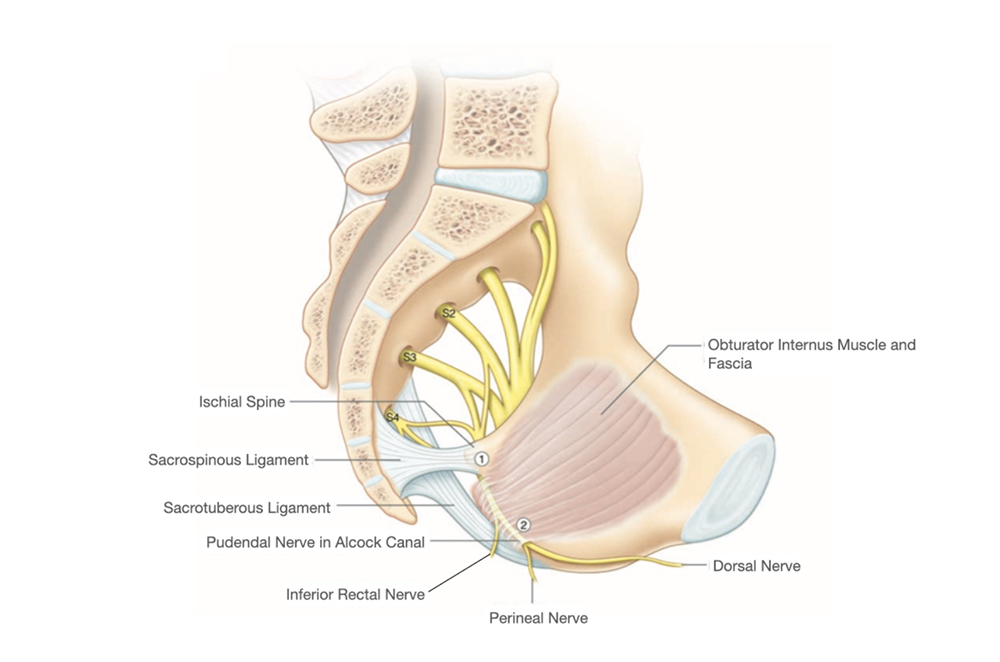
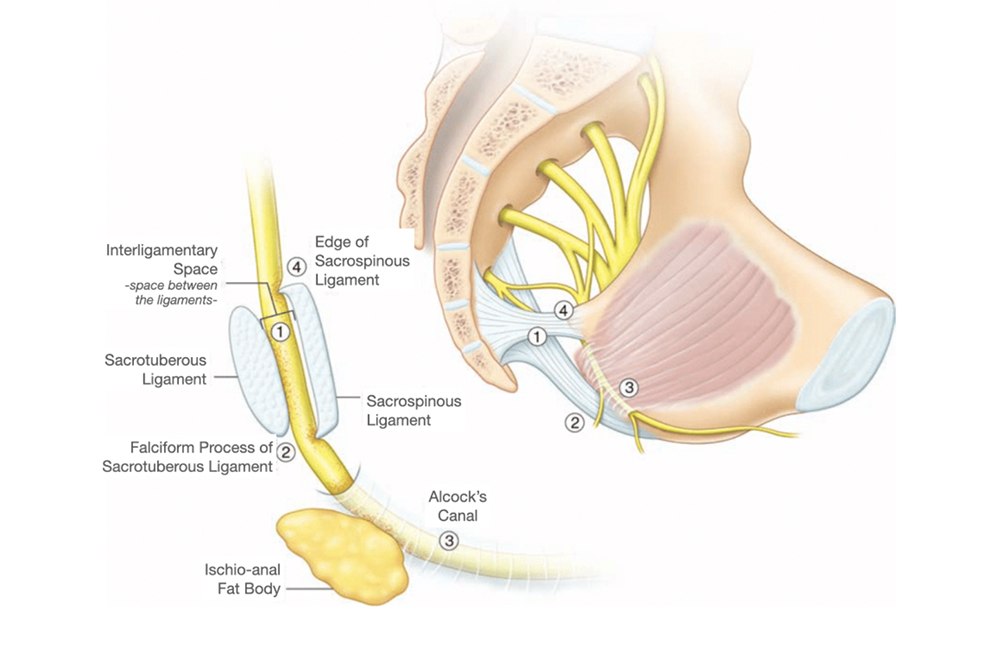
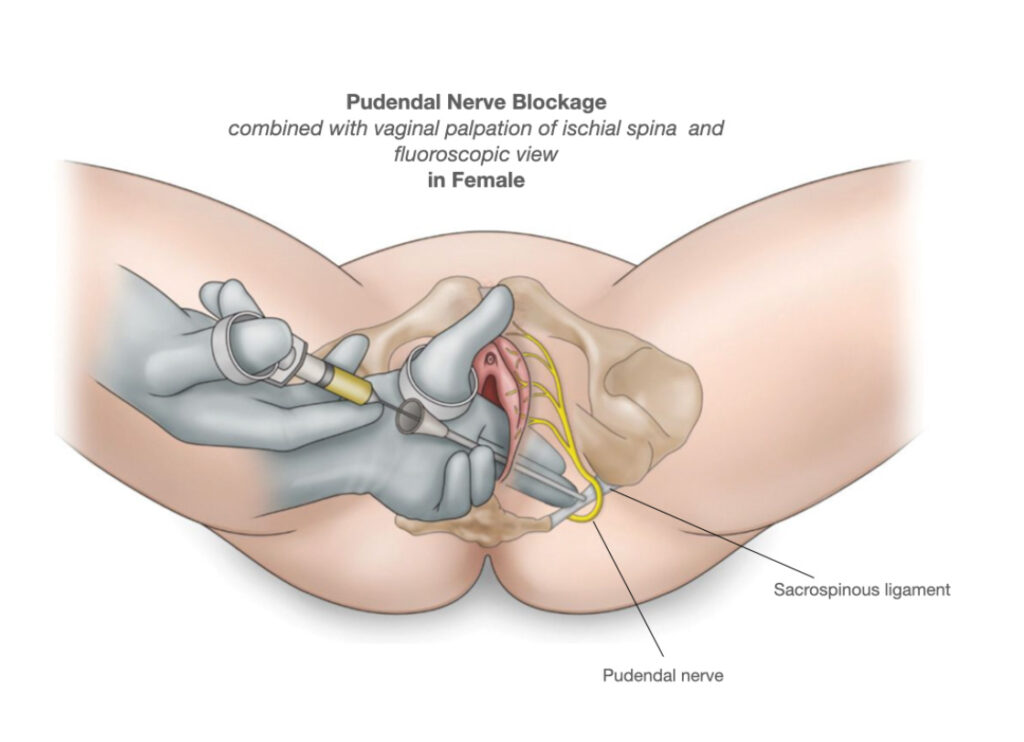
Comparison with quadrupeds, the bipedal body shape of humans requirements a strong pelvic floor muscles and a well-developed ischial spine. With bipedal movements, traction by ligaments and fascias remodel the ischium, the ischial spine. Bony changes are consistently evident during pudendal blocks under fluoroscopic view. The remodeled ischial spine projects medially, superiorly, and posteriorly. The tip of spina can become broad and rounded bilaterally. Unilateral ischial spina remodeling occurs in equestrians and in athletes pushing off consistently with the same leg. Whilst ischial spina have sharp edges, the attached sacrospinous ligament broadens and rotates. The interligamentary space, between sacrospinous (SSL) and sacrotuberous (STL) ligaments, narrows and restricts nerve movement or causes compression. Sitting position compresses the nerve between the SSL and STL ligaments as “clamp”, probably causing ischemia. In addition, the ischioanal fat body may elevate the nerve against the falciform process of the sacrotuberous ligament.
Most surgical compressions (about 90%) are found between the STL and SSL ligaments (the interligamentous space). Multiple fascial bands may compress the nerve near the ischial spine. About 10% of compressions are observed in the pudendal (Alcock’s) canal.
Symptoms and Signs
The mostly main symptom is a burning or stabbing pain in the perineum, the area between the anus and genitals (anogenital region), which often gets worse when sitting or driving and eases when standing or lying down. Other symptoms might include numbness of the same area, difficulty with bladder or bowel control, and genital pain during sexual activity. Causes can vary, from sitting for long periods, like cycling, to pelvic trauma, surgeries, or even tumors pressing on the nerve.
Pudendal Nerve Entrapment Syndrome (PNES) is a complex and often underdiagnosed condition that significantly impacts quality of life. This detailed review examines the anatomy and pathophysiology of the pudendal nerve, the clinical presentation of pudendal neuralgia, diagnostic challenges, and the full spectrum of treatment options. A particularly innovative and effective surgical treatment—Robotic Surgery in Pudendal Neurolysis (also known as Robotic Pudendal Nerve Decompression Surgery)—has been pioneered by Prof. Dr. Tibet Erdogru. For further detailed information about this groundbreaking procedure, please click the following link: [LINK].
Differantial Diagnosis
Symptoms or signs of some pelvic syndromes harvested by different disciplines may be caused by pudendal neuropathy. Publications in the literature regarding the syndromes and each of the differential diagnoses below do not define or rule out pudendal neuropathy.
In some of the patient
chronic pelvic pain syndrome (titled as chronic non bacterial prostatitis) only conventional
The simple pinprick sensory examination is not described in any clinical research articles on CPP. Only conventional morphologic and infectious causes of pelvic pain are considered. Other processes may affect the same symptoms. Neurologists typically consider herniated intervertebral disk and multiple sclerosis. Tarlov cysts are occasionally identified on MRIs. In our experience, the cysts did not contribute to CPP (N > 20). This is shown definitely because pudendal blocks distal to the Tarlov cyst consistently relieved the pain/symptoms. Urologists diagnose prostatitis and varicocele. Gynecologists may call the symptoms endometriosis, ovarian cyst (rupture, torsion), ovarian vein syndrome, or ves- tibulitis. Physical therapists diagnose myofascial dysfunctions and trigger points.
Diagnosis of Pudendal Nerve Entrapment
Diagnosis is complex due to symptom overlap with other conditions like pelvic floor dysfunction or prostatitis. The “Nantes criteria,” established in 2006, are crucial for diagnosis, including:
Criterion | Description |
Pain Distribution | Pain in the pudendal nerve area (perineum, genitals, anus). |
Pain Aggravation | Predominantly experienced while sitting. |
Sleep Impact | Pain does not wake the patient from sleep. |
Sensory Impairment | No objective sensory loss, except possible allodynia. |
Nerve Block Response | Pain relieved by a pudendal nerve block. |
Introduction
Pudendal Neuralgia, characterized by chronic pelvic pain and a range of debilitating symptoms, is often associated with entrapment or irritation of the pudendal nerve. Patients typically present with pain in the perineal, genital, or pelvic regions, which may worsen with sitting or certain movements. Despite its prevalence, the diagnosis and management of this condition remain challenging due to its multifactorial etiology and variable clinical presentation.
Anatomy and Physiology
The pudendal nerve originates from the sacral plexus (S2–S4) and courses through the pelvic region, providing sensory, motor, and autonomic innervation to the perineum. Its pathway through the greater sciatic foramen, around the ischial spine, and into the pudendal canal (Alcock’s canal) renders it vulnerable to compression or entrapment by surrounding anatomical structures or pathological conditions.
Pudendal Neuralgia vs. Pudendal Nerve Entrapment
While the terms are sometimes used interchangeably, it is important to differentiate:
- Pudendal Neuralgia refers broadly to chronic pelvic pain related to the pudendal nerve.
- Pudendal Nerve Entrapment Syndrome specifically implies that the nerve is being compressed or entrapped, leading to neural irritation and pain.
Understanding this distinction is essential for tailoring effective treatment strategies.
Causes and Risk Factors
Pudendal nerve entrapment can result from a variety of factors, including:
- Anatomical variations or congenital anomalies.
- Trauma or surgical complications, such as pelvic surgeries that may inadvertently affect the nerve.
- Prolonged mechanical pressure, often seen in cyclists or individuals who spend extended periods sitting.
- Inflammatory conditions and scar tissue formation.
- Childbirth-related injuries that may contribute to nerve compression.
A thorough patient history and clinical evaluation are vital in identifying these causative factors.
Clinical Presentation and Symptoms
The hallmark symptoms of PNES include:
- Chronic pelvic pain that is often described as sharp, burning, or stabbing.
- Pain exacerbation during prolonged sitting or physical activities.
- Sensory disturbances such as numbness or tingling in the genital or perineal areas.
- Sexual dysfunction or urinary difficulties in some cases.
These symptoms can severely impact daily activities and quality of life, underscoring the importance of prompt and accurate diagnosis.
Treatment Modalities
Conservative Management
Initial treatment strategies often include:
- Physical Therapy: Focused on pelvic floor rehabilitation and posture correction.
- Medications: Including analgesics, anti-inflammatory drugs, and neuropathic pain agents.
- Lifestyle Modifications: Ergonomic adjustments and activity modifications to reduce pressure on the pudendal nerve.
- Interventional Procedures: Such as nerve blocks or trigger point injections, which can offer temporary relief.
Surgical Intervention:
Robotic Surgery in Pudendal Neurolysis
For patients who do not respond adequately to conservative management, surgical intervention may be indicated. Among the available techniques, Robotic Surgery in Pudendal Neurolysis stands out due to its precision and minimally invasive nature. This procedure, also known as Robotic Pudendal Nerve Decompression Surgery, is performed by Prof. Dr. Tibet Erdoğru and represents a significant advancement in the treatment of PNES.
Procedure Overview:
- Minimally Invasive Approach: Utilizing robotic assistance, the surgeon gains enhanced visualization and precision in navigating the complex pelvic anatomy.
- Targeted Decompression: The procedure involves the careful dissection and decompression of the pudendal nerve, thereby relieving the entrapment and mitigating the associated neuralgic pain.
- Enhanced Recovery: The robotic approach minimizes tissue trauma, leading to reduced postoperative pain and quicker recovery times compared to traditional open surgery.
Prof. Dr. Tibet Erdoğru’s expertise and innovative application of robotic technology have markedly improved outcomes for patients suffering from PNES. For more detailed information about this state-of-the-art treatment, please click the: [LINK].
Pioneering Laparoscopic Innovations by
Prof. Dr. Tibet Erdoğru
Prof. Dr. Tibet Erdoğru, M.D. has been a trailblazer in the evolution of pudendal nerve surgery. His pioneering contributions include:
- Laparoscopic Pudendal Nerve Decompression (2014): Prof. Erdoğru was the first in the world to describe a laparoscopic approach for pudendal nerve decompression. This milestone—the first clinical laparoscopic pudendal surgery in the literature—marked a significant advancement in minimally invasive pelvic surgery. For further reading, please visit: https://pubmed.ncbi.nlm.nih.gov/24149853/.
- Laparoscopic Pudendal Neurolysis in Pelvic Mesh Surgery: He also was the first to describe laparoscopic pudendal neurolysis in patients with Pudendal Nerve Entrapment due to pelvic mesh surgery. For detailed information, please click here: https://pubmed.ncbi.nlm.nih.gov/27250921/.
- Laparoscopic Selective Pudendal Nerve Neuromodulation in Neurogenic Bladder: Further extending his innovative approach, Prof. Erdoğru introduced laparoscopic selective pudendal nerve neuromodulation as a treatment modality for neurogenic bladder. More details can be found here: https://pubmed.ncbi.nlm.nih.gov/32395321/.
These groundbreaking laparoscopic and robotic techniques have expanded the therapeutic options for patients and continue to influence modern surgical practice in the management of PNES.
Future Directions and Research
Ongoing research into the pathophysiology and treatment of PNES is essential. Future studies are expected to refine diagnostic criteria, enhance surgical techniques, and explore novel therapeutic avenues. Emphasis on multidisciplinary collaboration and patient-centered care will continue to drive improvements in outcomes.
Pudendal Nerve Entrapment Syndrome is a multifaceted condition requiring comprehensive evaluation and a tailored treatment approach. With a range of conservative and surgical options available, the innovative robotic neurolysis procedure performed by Prof. Dr. Tibet Erdoğru offers new hope for patients with refractory symptoms. Early diagnosis and prompt intervention are crucial to improving quality of life, and ongoing research will undoubtedly further enhance our management strategies.
For more detailed information on the innovative Robotic Surgery in Pudendal Neurolysis performed by Prof. Dr. Tibet Erdoğru, please click here: [LINK].
Robotic Surgery in Pudendal Neurolysis:
A Detailed Look
This procedure, performed using systems like the da Vinci Surgical System, provides a 3D high-definition view and wristed instruments for precise maneuvers in the pelvic area. The steps include:
Step | Description |
Patient Positioning | Placed in low-lithotomy with steep Trendelenburg for pelvic access. |
Port Placement | Small incisions (3 incision, 8 mm in each) for robotic arms and camera insertion. |
Dissection | Identification of the pudendal nerve, pudendal artery, pudendal vein asi pudendal neurovascular bundle and compressing structures, like ligaments, muscles. |
Neurolysis | Incision or removal of compressing structures to free the nerve, artery and vein. |
Closure | Incisions closed, patient fastly recovered with no surgical pain |
Advantages include enhanced visualization, reduced blood loss, shorter hospital stays, and faster recovery, as detailed in Prof. Dr. Tibert Erdoğru’s Robotic Surgery Page. Prof. Dr. Tibert Erdoğru, a urologist with extensive experience, pioneered laparoscopic pudendal nerve decompression in 2014 and transitioned to robotic methods since 2021, with publications supporting its efficacy. His work includes case reports showing 90% pain reduction sustained at 10 weeks post-procedure.
Pudendal Nerve Entrapment Syndrome requires a multidisciplinary approach, with conservative treatments as the first line and robotic surgery as an effective option for non-responders. Prof. Dr. Erdoğru’s advancements in robotic pudendal neurolysis offer hope for improved outcomes, emphasizing precision and minimal invasiveness.
For those experiencing symptoms and seeking advanced treatment, contact Prof. Dr. Tibert Erdoğru’s clinic for a consultation to explore Robotic Pudendal Nerve Decompression Surgery. You can also follow the robotic pudendal nerve releasing videos via LINK.
