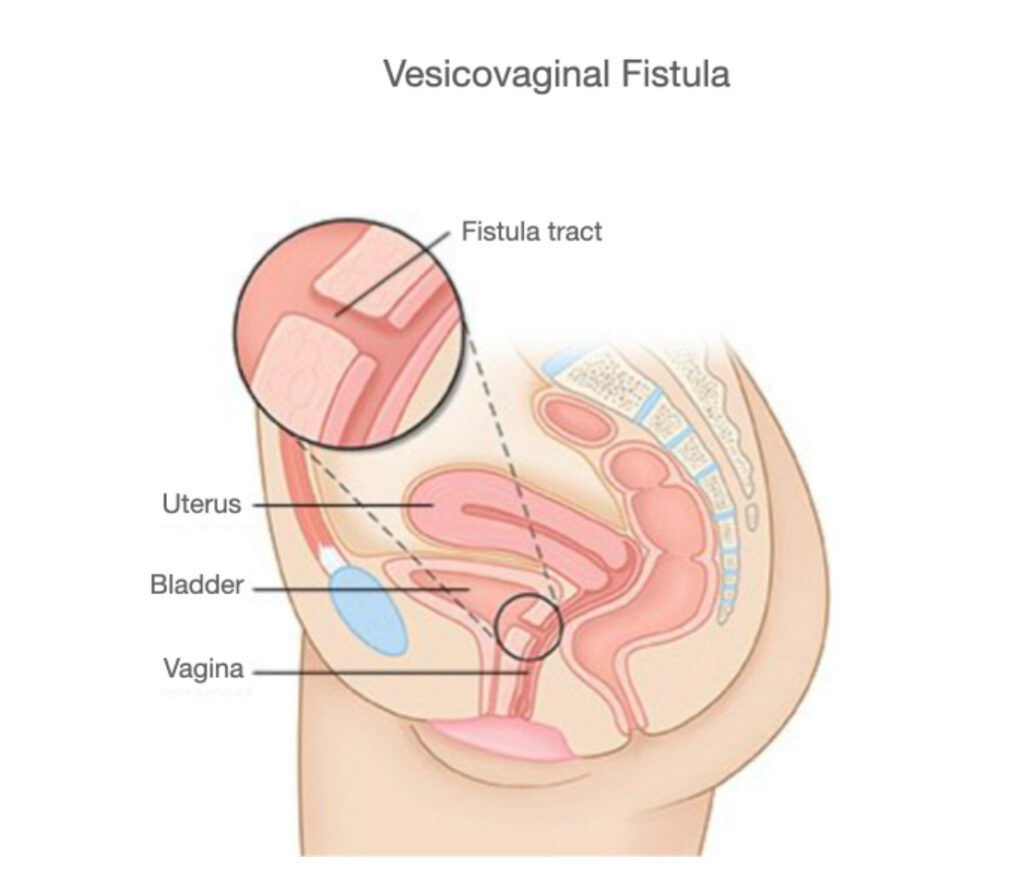
What is the mean of fistula?
A fistula is a passage of channel which formed
between two hollow organs in your body (veciovaginal fistula means fistula channel between urinary blşadder and vagina) or
between a hollow organ and your skin (vesicocutaneous fistula means fıstula channel between urinary bladder and skin)
The main symptom is involuntary urinary leakage from the vaginal vault, resulting in skin irritation, recurrent urinary tract infections.
Diagnostic Evaluation:
* Pelvic examination to determine the fistula tract on the vaginal side. If it is small or deeply posterior, after metilen blue injection into the bladder, an inserted vaginal swab turns blue
* Cystoscopy combined with retrograde pyeloureterography if there is risk for ureterovaginal fistula
* Voiding cystography to identify and locate the fistula and its diameter
* Abdominal MRI or CT scan to rule out ureteral injury and to search for pelvic pathologies.
What do I need to know about a VVF repair?
When VVF is large or doe not respond to conservative approaches as prolonged urinary bladder cahteterization, surgical correction is indicated with a success rate of 76-97% in patients of fistula resulting in surgical injury. Vesicovaginal fistula repair is surgery to remove fibrotic fistula tract and separately closing of bladder and vaginal walls. Different surgical techniques have been proposed for repair of VVF depending on the etiology, location and diameter of fistula, surgeon’s experience.
Although the morbidity of open abdominal repair is significant compared with that of the vaginal approach (despite especially familiar for gynecologist), abdominal approach is usually preferred in patients with
* A large (>2 cm diameter) or supratrigonal fistula
- Fistula close proximity to ureteral orifices
especially in patients with previous or multiple complicated transvaginal or transabominal VVF repairs.
With surgeon experience in advanced reconstructive robotic surgery, to decrease the morbidity of the abdominal approach, a repair with robotic surgery is the most effective approach which is primarily associated with better success rates, minimal surgical trauma and lesser morbidity, thus allowing more rapid convalescence.
Certain indications for abdominal & robotic surgery approach:
* Inadequate exposure related to a high or retracted fistula in a narrow vagina
* Close proximity of the fistula to the ureter
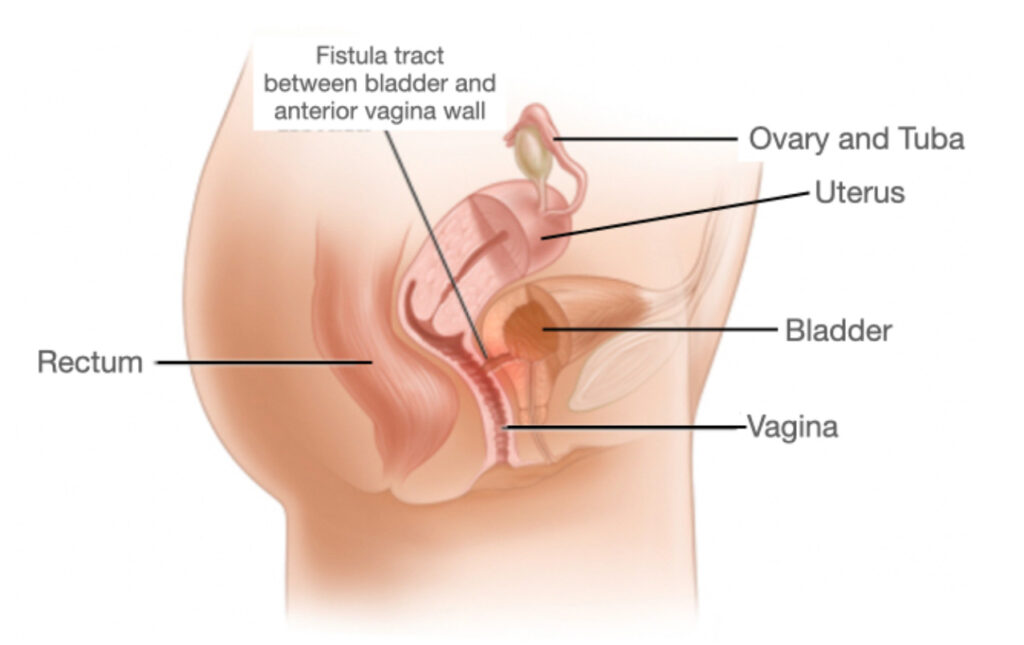
* Together with another pelvic pathology as ureteric injury (ureterovaginal fistula*) or a complex fistula involving another intraabdominal organ
* Multiple fistulae
- Previously failed transvaginal or open abdominal repair attempt
Robotic Surgery Steps for VVF Repair
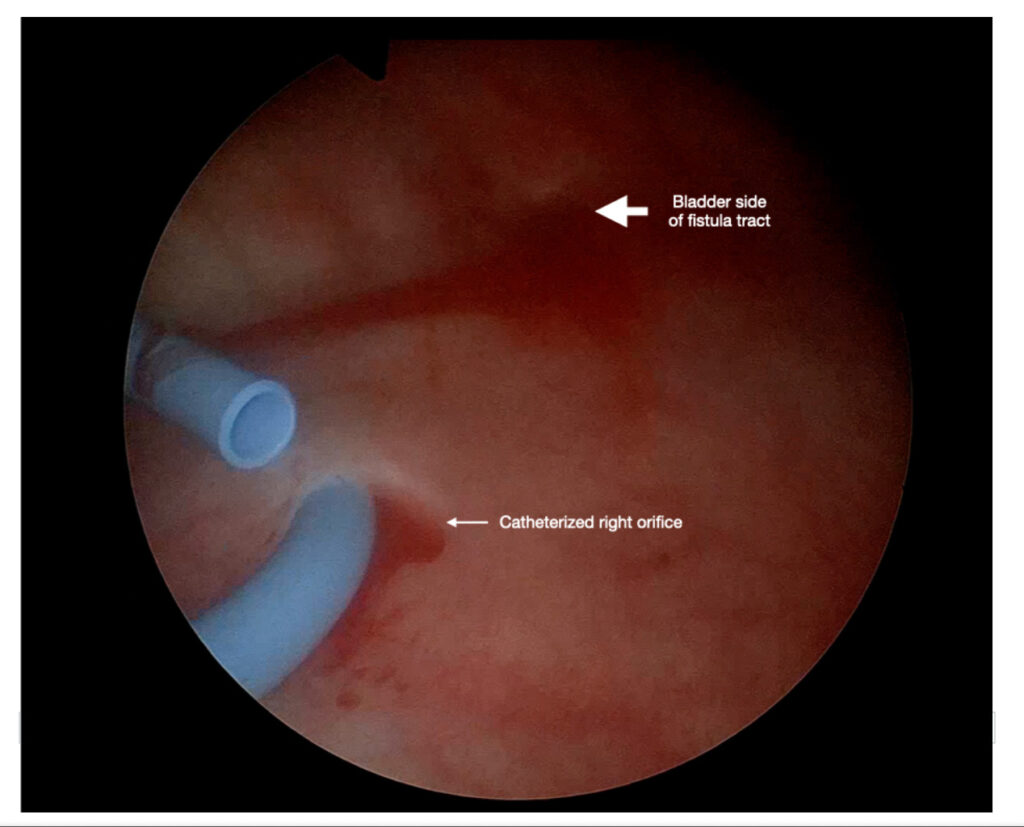
Cystoscopy is performed combined with retrograde pyelography if there is risk for ureterovaginal fistula, and two ureters are catheterized using JJ stent. Thus ureter identification and protection during excision of fistula tract and closure of the walls are guaranteed (Figure-3).
The main symptom is involuntary urinary leakage from the vaginal vault, resulting in skin irritation, recurrent urinary tract infections.
Diagnostic Evaluation:
* Pelvic examination to determine the fistula tract on the vaginal side. If it is small or deeply posterior, after metilen blue injection into the bladder, an inserted vaginal swab turns blue
* Cystoscopy combined with retrograde pyeloureterography if there is risk for ureterovaginal fistula
* Voiding cystography to identify and locate the fistula and its diameter
* Abdominal MRI or CT scan to rule out ureteral injury and to search for pelvic pathologies.
What do I need to know about a VVF repair?
When VVF is large or doe not respond to conservative approaches as prolonged urinary bladder cahteterization, surgical correction is indicated with a success rate of 76-97% in patients of fistula resulting in surgical injury. Vesicovaginal fistula repair is surgery to remove fibrotic fistula tract and separately closing of bladder and vaginal walls. Different surgical techniques have been proposed for repair of VVF depending on the etiology, location and diameter of fistula, surgeon’s experience.
Although the morbidity of open abdominal repair is significant compared with that of the vaginal approach (despite especially familiar for gynecologist), abdominal approach is usually preferred in patients with
* A large (>2 cm diameter) or supratrigonal fistula
- Fistula close proximity to ureteral orifices
especially in patients with previous or multiple complicated transvaginal or transabominal VVF repairs.
With surgeon experience in advanced reconstructive robotic surgery, to decrease the morbidity of the abdominal approach, a repair with robotic surgery is the most effective approach which is primarily associated with better success rates, minimal surgical trauma and lesser morbidity, thus allowing more rapid convalescence.
Certain indications for abdominal & robotic surgery approach:
* Inadequate exposure related to a high or retracted fistula in a narrow vagina
* Close proximity of the fistula to the ureter
* Together with another pelvic pathology as ureteric injury (ureterovaginal fistula*) or a complex fistula involving another intraabdominal organ
* Multiple fistulae
- Previously failed transvaginal or open abdominal repair attempt
Robotic Surgery Steps for VVF Repair
Cystoscopy is performed combined with retrograde pyelography if there is risk for ureterovaginal fistula, and two ureters are catheterized using JJ stent. Thus ureter identification and protection during excision of fistula tract and closure of the walls are guaranteed (Figure-3).
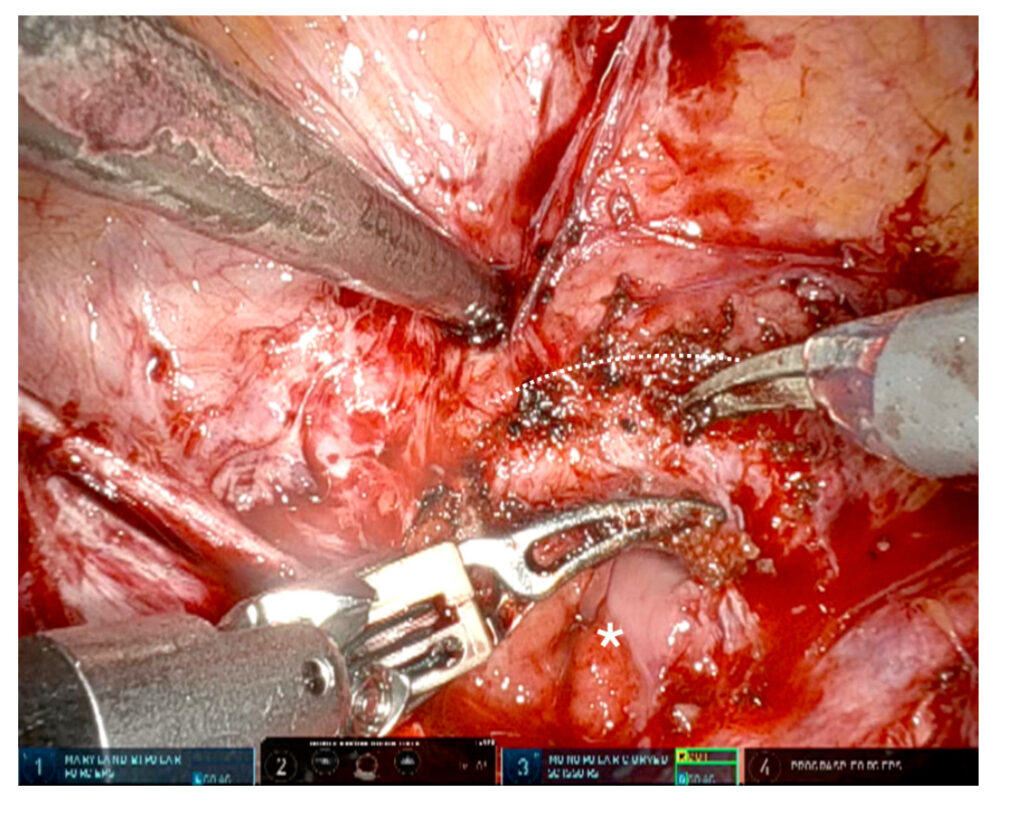
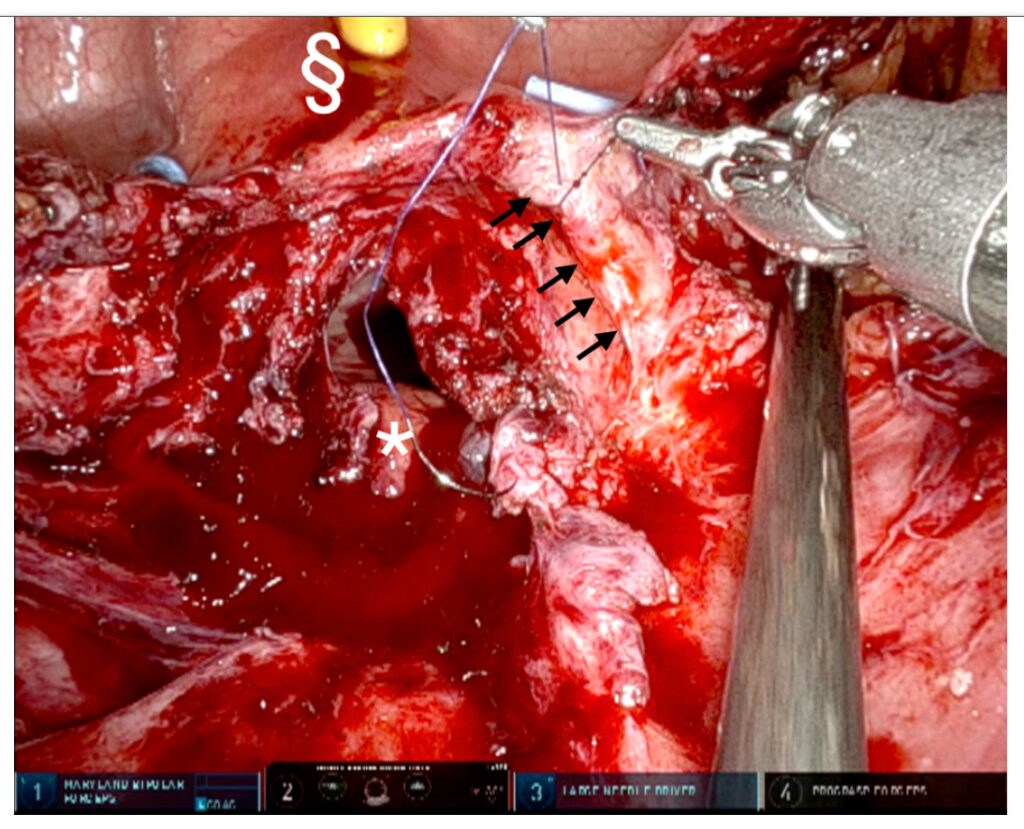
Severe scar tissue between the vagina and bladder due to previous surgeries are sharply dissected after filling the bladder with 60-90 cc saline. In the Figure-4, vaginal opening due to severe scar tissue (white star) and severe adhesion (white dotted line).
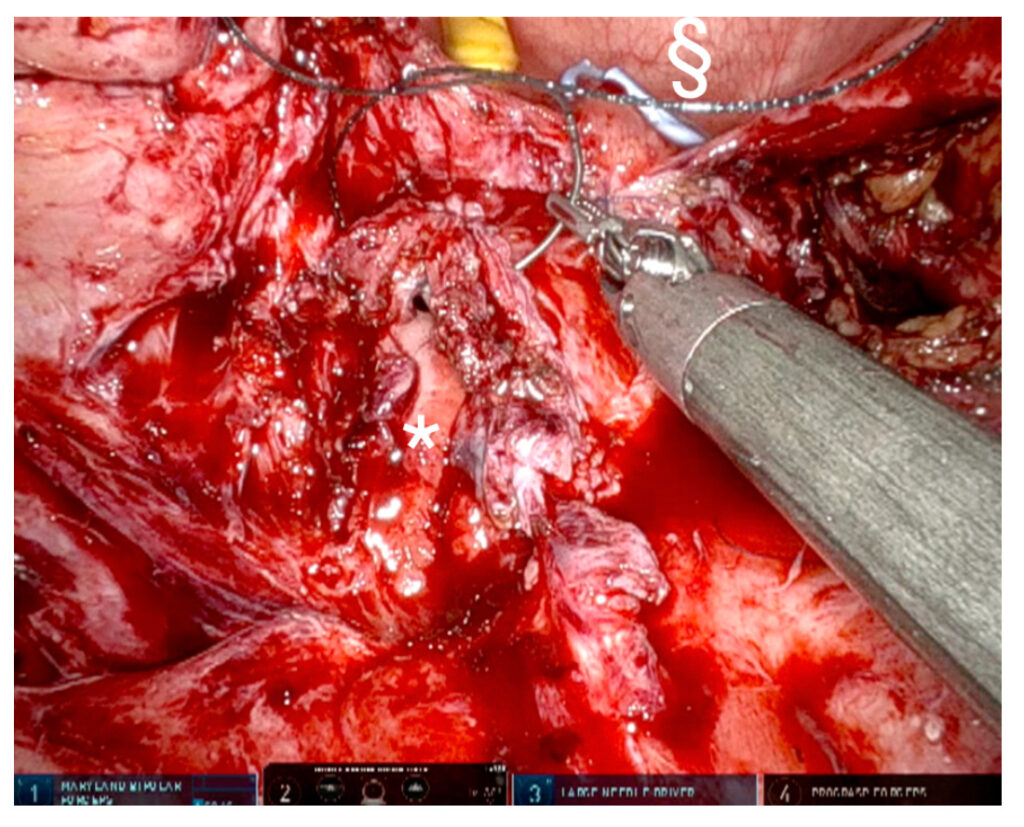
After completely dissection of scar tissue and fistula tract, all these are removed and healthy tissues should be determined because of higher success rate. Right ureteral-vaginal fistula can be identified, especially in previous traumatic surgeries, and repaired using 5-0 Vicryl separately (Figure-5). This robotic surgery can be followed at Prof. Dr. Tibet Erdogru’s Youtube Channel
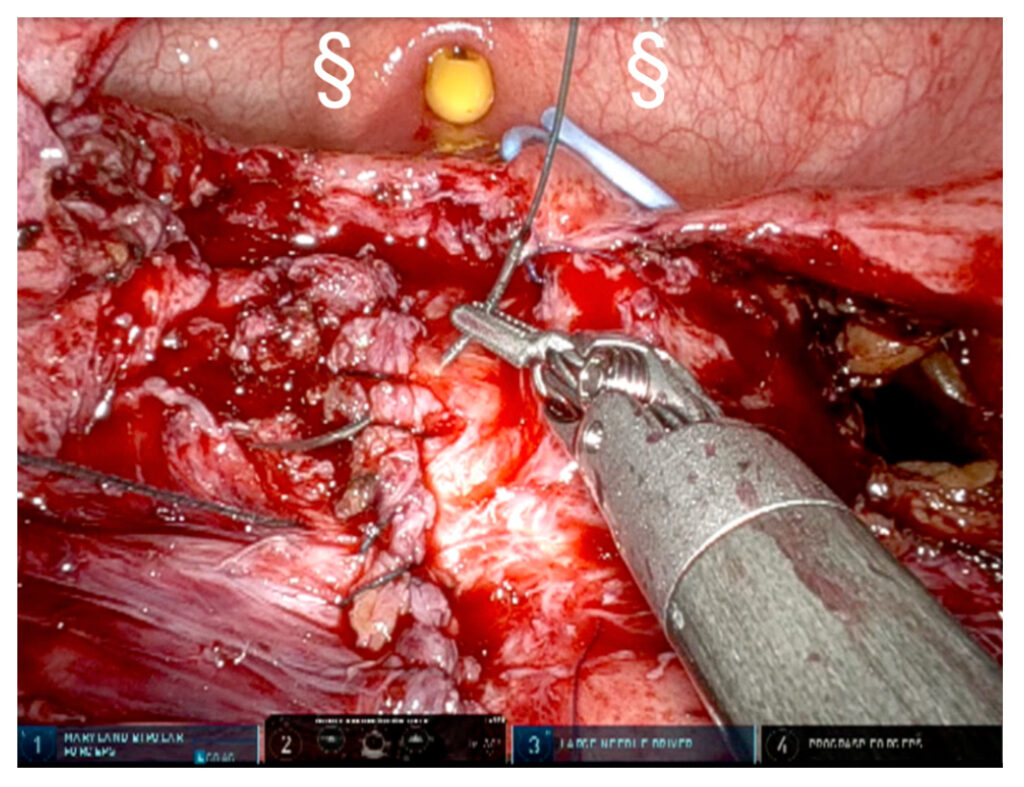
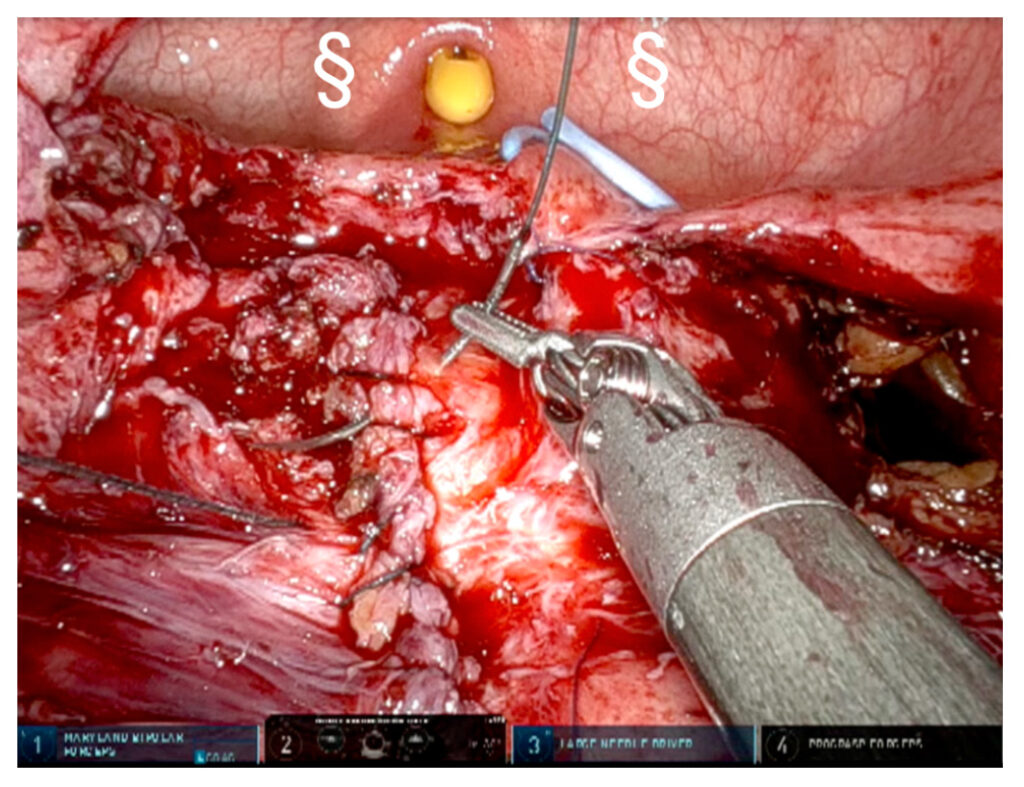
Vaginal anterior wall is closed using 3-0 V-lok suture with two layers, that can be observed in Figure-6a and Figure-6b.
Before or after closure of bivalved bladder wall, Omentum flap as two layers is placed between the vagina and bladder to secure blood supply and vascularized barrier (Figure-7). After mental flap fixing over the vaginal repair line, bladder wall is closed using 3-0 V-lok sutures after changing ureteral stents with single J 7 Fr catheters.
Care After Surgery and Follow-up
After surgical patient care of robotic surgery in VVF repair is not different from that of the open surgery.
- The drain removed 1 or 2 days after the surgery if drainage is less than 50 ml in a day. The patient is discharged home with and bladder Foley catheter and two single J ureteric catheter. Because of our experience, insertion of the single J ureteral single J stents is beneficial mostly because the bladder remains almost completely dry to facilitate the healing process of vaginal and bladder walls. Thus, they remain in place for 7 days.
- Urethral Foley catheter is removed on postoperative days 14-21 control with or without cystography, depending on the quality of reconstruction and surgeon’s preference. Cystography is not always mandatory. Patients warned to be cautious not to use intravaginal tampons and avoid sexual intercourse for 2 months.
- Postoperative prophylactic antibiotics are usually prescribed until all catheters are removed. After removal of urethral catheter, any urinary tract infection must be treated.
Prof. Dr. Tibet Erdogru
Uro-Klinik – Istanbul
